What is heart failure?
Heart failure means the heart cannot keep up with the demands on it, particularly the heart’s inability to pump blood with usual efficiency.
It may result from the failure of right or left or both ventricles.
Or it may result from either the pump failure due to weak heart muscles or heart muscles fail to relax to receive the blood before it pumps.
For various reasons, the blood flow to the heart and body slows down, and the heart’s pressure increases. As a result, the heart cannot pump enough oxygen and nutrients to satisfy the body’s needs.
The heartbeat can stretch to prevent more blood from flowing through the body or respond by tightening and thickening.
.As a result, the kidneys respond to the body’s ability to store water (fluids) and salt. When fluid builds up in the hands, feet, ankles, feet, lungs or other parts of the body – a condition known as congestive heart failure (CHF).
A congestive heart attack is a severe progressive condition that alters the heart’s muscle ability to pump blood. Although it is commonly referred to as heart failure, congestive heart attack describes explicitly a phase in which fluids accumulate around the heart and renders it inefficient in pumping blood.
Congestive heart failure occurs when the ventricles are unable to pump adequate blood into the body. As a result, blood and other fluids accumulate in the lower body, liver, stomach and lungs. The condition is severe and requires you to seek instant medical assistance.
Symptoms of heart failure.
During the early stages, you are less likely to detect any complications in your health. However, as your condition progresses, you will notice significant changes in your body.
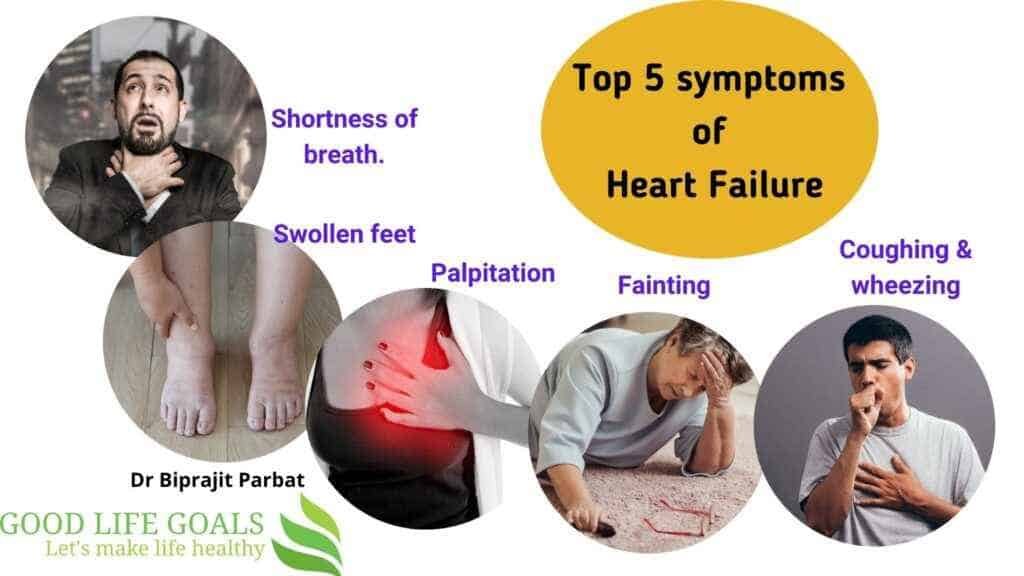
Heart failure initial symptoms
- a Heightened urge of urinating particularly at night
- Weight gain
- Swollen legs, ankles and feet
- Fatigue
Symptoms indicating your condition has worsened.
- Shortness of breath points out pulmonary oedema where excess fluids accumulate in your lungs and require immediate medical attention.
- Wheezing
- Coughing due to congested lungs
- Irregular heartbeat
Symptoms indicating a severe heart condition
- Fainting
- Blue skin as a result of insufficient oxygen in the lugs
- Rapid breathing
- Chest pains radiating via the upper part of the body
Relevant statistics of heart failure –
In 2015, over 40 million individuals were reported to have heart failure globally.
In general, 2% of adults have heart failure, and the rate ranges between 6% to 10% for individuals over 65 years.
Above the age of 75, heart failure rates are higher than 10%.
Heart failure rates are expected to increase. The increase in the rates is major due to prolonged lifespan and high survival rates from other types of cardiovascular illnesses and increased risk factors, specifically obesity, diabetes, and hypertension. Heart failure remains the foremost cause of hospitalization for individuals over the age of 65 years.
United States
In the US, 5.8 million people are affected by heart failure, and 550,000 new cases are diagnosed annually. The disease was the leading cause of hospitalization for people aged 85 years and above and the second-most common for people aged between 65 to 84 years in 2011.
It is estimated that 1 out 5 adults develop heart failure at the age of 40 years and about half of them die within 5 years of diagnosis.
Heart failure is more prevalent among Native Americans, Hispanics, and African Americans and is associated with high hypertension and diabetes cases in these ethnic groups. New immigrants from the Eastern Block nations like Russia are also greatly affected by heart failure and associated with inadequate preventive health care.
- Readmission of 1 out of 4 (24.7%) cases of heart failure hospitalization in the United States happens within 30 days.
- Also, more than 50% of heart failure patients seek readmission within 6 months, with an average hospital stay of 6 days.
- Heart failure is the major cause of hospital readmissions in the United States. 24.5 % out 100% of individuals aged 65 and above diagnosed with heart failure were readmitted in 2011.
United Kingdom
Despite the significant improvements in heart failure risk factors prevention in the UK, the rates have continued to rise as a result of ageing factor and population increase. In general, heart failure rates are similar to the four leading causes of cancer, i.e. colon, prostate, lung and breast combined.
Developing countries
Valvular heart disease is the leading cause of heart failure in tropical countries. As developing nations have become more affluent, the cases of obesity, hypertension and diabetes are on the rise, which has increased the number of people affected by heart failure.
Types of heart failure
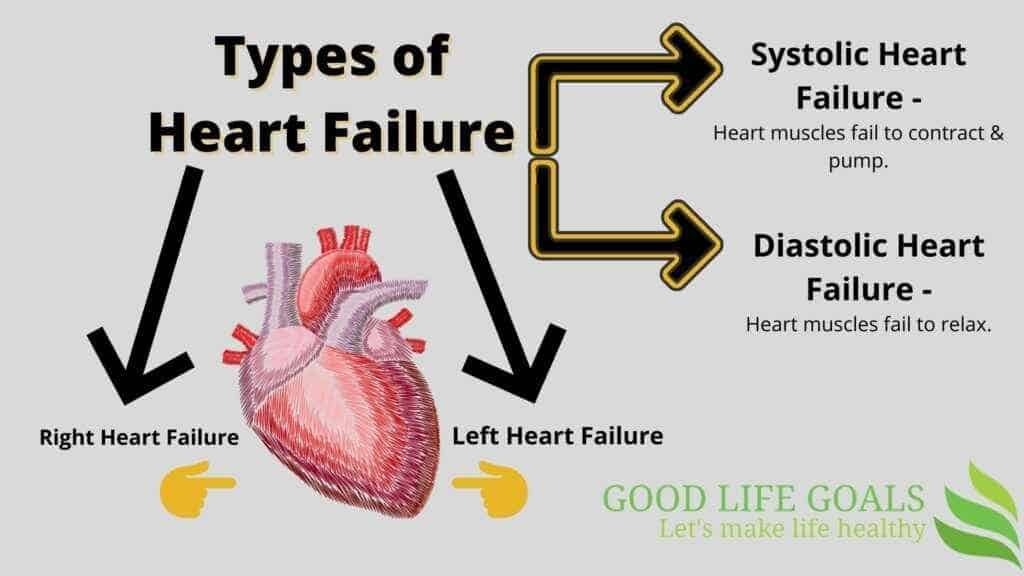
Left-sided failure
The heart’s left side carry oxygenated blood and transport it to all parts of the body except pulmonary circulation. In Left-sided heart failure, blood accumulates in the lungs, causing fatigue and respiratory symptoms due to insufficient oxygen and blood supply.
During this type of heart failure, an individual experiences rapid breathing, Crackles that point out pulmonary oedema and cyanosis manifest as a late symptom of severe pulmonary oedema. Other symptoms include irregular heartbeats and heart murmurs which is a sign of valvular heart disease. There are two types of left-sided heart failure:
Heart failure with reduced ejection fraction (HFrEF) described as a systolic failure.
The left ventricle is unable to contract normally causing the heart inefficiency to pump adequate blood into circulation.
Heart failure with reduced ejection fraction (HFpEF) described as a diastolic failure.
The left ventricle is unable to relax normally. The heart cannot be correctly filled with blood in between the resting period of every beat.
Backward failure of the left ventricle leads to blood accumulation in the lung’s blood vessels and is manifested through respiratory symptoms. This type of heart failure can be grouped into the failure of left atrium or ventricle or both within the left chamber.
An individual experiencing backward failure will develop dyspnea at rest and shortness of blood. Elevated breathlessness on lying flat also happens and is normally examined based on how many pillows are needed to lie comfortably. The left ventricle’s forward failure may lead to signs of poor disrupted systematic circulation like confusion and dizziness.
Right-sided failure
Here the right side heart fails to pump blood to the lungs. It may happen due to heart muscle weakness, heart attack or heart valve issues.
This type of heart failure is normally resulting from pulmonary heart disease, which is brought about by difficulties of pulmonary circulation like pulmonic stenosis and pulmonary hypertension.
An individual with right-sided failure may experience spleen and liver enlargement, ascites and indentation of peripheral edema.
Backward failure of the right ventricle causes accumulation in the systematic capillaries.
This produces an excess amount of fluids in the body resulting in swelling around the foot and ankles.
Increased urge to urinate during the night happens when the legs’ fluid is reversed to the bloodstream while lying down.
In serious cases, liver enlargement and ascites may occur. If left untreated progressive liver congestion may lead to liver damage as well as blood clotting related problems.
Biventricular failure
The lung’s inefficiency in finger percussion and diminished breath sounds at the lung’s bases may indicate a pleural effusion (collection of fluid between the chest wall and the lung). Although it can happen in separated left or right-sided heart failure, it is more prevalent in biventricular failure given that pleural veins drain into both pulmonary and systematic venous systems.
As an individual with an isolated ventricle heart failure continues to live; it advances both ventricles’ failure. For instance, left ventricle failure leads to pulmonary hypertension and pulmonary oedema, which in turn elevates stress on the right ventricle. Although it’s not harmless, right ventricle heart failure is not as injurious to the other side.
High-output heart failure
Heart failure may happen in high output cases where an abnormal amount of blood is pumped such that the heart cannot keep up. This can result from overload cases such as arteriovenous malformations, chronic severe anemia and kidney diseases.
How heart failure is diagnosed?
Early diagnosis and treatment may assist individuals with heart failure to live longer and more active lives.
Family and medical histories
- Information about the following are important –
- Diabetes
- Blood pressure
- Already having a heart problem or heart attack.
- Thyroid issues,
- Cholesterol issues,
- Smoking,
- Family h/o.
Body signs of heart failure –
- Irregular heartbeats,
- swollen abdomen, legs, feet & ankles and
- Swollen veins around the neck.
Diagnostic tests for heart failure –
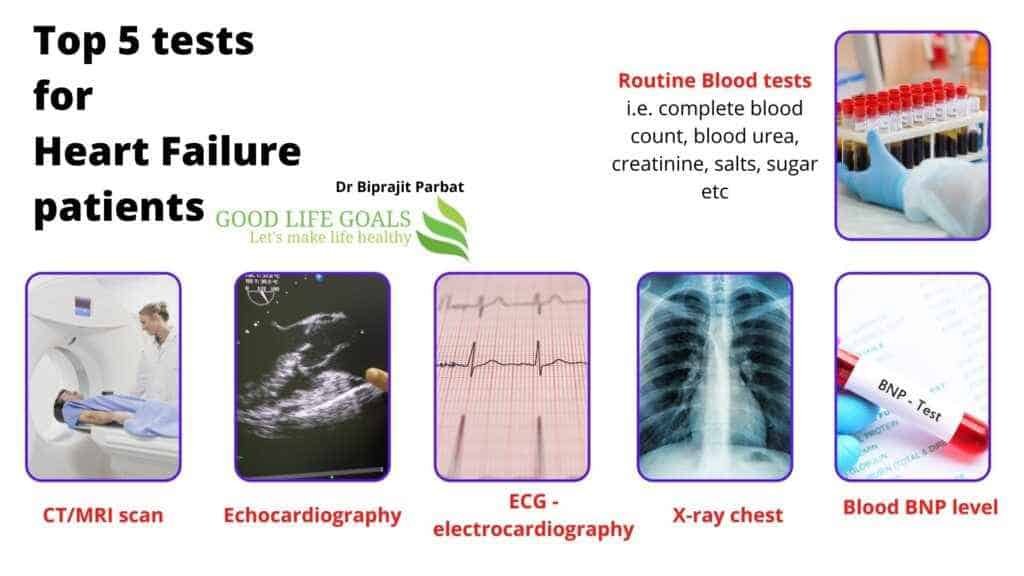
EKG (Electrocardiogram) –
This is a painless, simple test that measures and records the electrical activity of the heart. The test reveals how your heartbeat and identifies whether you have a steady or an irregular rhythm. It also shows the timing and strength of electrical signals passing through your heart. An electrocardiogram may help identify the thickness of your heart’s pumping chamber walls. Abnormally thicker walls make it extra hard for the heart to pump blood. The test can be used to reveal symptoms of a previous or a present heart attack.
Chest X-ray
A chest Xray is used to take photos of organs and tissues inside your chest like blood vessels, lungs, and hearts. The test results can be used to evaluate pulmonary congestion, heart size and alternative cardio-pulmonary illnesses that may result in an individual’s symptoms.
BNP blood test
BNP is a neurohormone found as secretory granules in both ventricles and less concentration in the atria. A BNP test is taken to examine the level of hormone present in your blood.
The level of this hormone elevates when you have a heart failure. This helps to know the disease severity and progression.
Biomarkers provide useful information as well as the level of severity of an ongoing heart failure.
The BNP value predicts death risk and cardiovascular problems in individuals previously diagnosed with heart failure. Increased BNP levels have been linked to chronic hypoxia, pulmonary hypertension, pulmonary embolism, and renal failure. People who are overweight have lower levels of BNP.
Transthoracic echocardiography (TTE)
This is the ultrasound of your heart and heart valves. This test shows the shape and the size of your heart and how efficient the heart’s chambers and valves work.
A two-dimensional echocardiogram with Doppler is used for the initial examination of individuals having heart failure. TTE detects valve function, ventricular function, wall motion and thickness.
Other methods include tricuspid valve regurgitant gradient combined with the examination of inferior vena cavil diameter and its functioning during respiration, which offers central venous and systolic pulmonary artery pressure estimates. Many of these abnormalities should be examined because they have a great predictive value in treating heart failure. Evaluation of ventricular function using TTE is effective when an individual has an acute decompensated heart failure.
Magnetic resonance imaging (MRI)
MRI test help evaluate left ventricle volume in comparison to that obtained using echocardiography. The additional information about fibrosis, viability, and myocardial perfusion obtained through MRI can help understand the cause of heart failure and evaluate outcome.
MRI gives a high anatomical resolution of all heart components and the surrounding structure; thus, it is highly preferred in known or suspected cardiovascular problems.
Computerized tomography (CT) scans
Cardiac CT scans give an accurate evaluation of heart structure and functioning even the coronary arteries.
However, both Cardiac CT and magnetic resonance imaging tends to be inaccurate in individuals with high heart rates.
The utilization of coronary angiography and cardiac catheterization are effective in individuals with new-onset angina and heart failure symptoms.
Predictors of poor outcome and high mortality rate in heart failure –
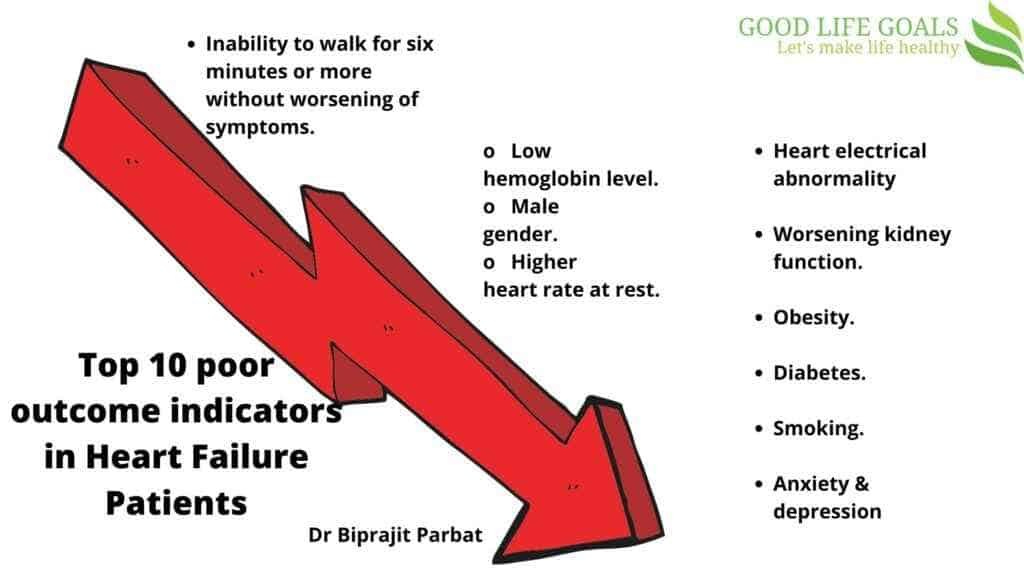
- Inability to walk for six minutes or more without worsening of symptoms.
- Low hemoglobin level.
- Male gender.
- Higher heart rate at rest.
- Heart electrical abnormality
- Worsening kidney function.
- Obesity.
- Diabetes.
- Smoking.
- Anxiety & depression.
Heart failure medications –
- Oxygen therapy.
- Fluid restriction to reduce intake of liquid mostly less than 1.5 liter per day.
- Diuretics to take out excess fluid load from the body,
- Angiotensin-converting enzyme (ACE) inhibitors (ACE-I) or angiotensin receptor blockers (ARBs) if the individual has a long-term cough as a side effect of the ACE-I. This is to reduce the action of body chemicals that worsen heart failure. Using medications from this class is linked with improved life quality, reduced hospitalizations, and improved survival for heart failure individuals.
- Beta blocker to reduce the death of heart muscle due to high sympathetic activity in heart failure patients.
For individuals with severe kidney dysfunction and ACE-I intolerance, a combination of long-acting nitrate and hydralazine has been identified as effective. It has been revealed to lower mortality in individuals with moderate heart failure. It is majorly effective in African-Americans.
A combination of ACE-I, beta-blockers, and mineralocorticoid antagonist can help lower mortality and improve symptoms for individuals with symptomatic heart failure characterized by low ejection fraction.
For individuals showing symptoms while still on mineralocorticoid receptor antagonist, beta-blockers and ACE-I, the risk of hospitalization or death due to heart failure can be lowered using valsartan/sacubitril.
Medications for chronic heart failure does not have a mortality benefit.
- Digoxin is one of them where its high toxicity and reduced therapeutic window has lowered its clinical practice significance. It only used on few individuals with refractory symptoms and have chronic hypotension or atrial fibrillation.
- Diuretics have been effective in treating fluid accumulation. Despite being widely used, evidence of their safety and effectiveness is limited in the absence of mineralocorticoid antagonists.
- Vasopressin receptor antagonists are also useful in heart failure treatment.
An automatic implantable cardioverter-defibrillator (AICD) has been shown to lower the mortality for individuals with reduced left ventricular ejection.
The primary goal of treatment is to improve heart failure symptoms and prevent the disease’s progression.
Heart failure treatment involves pharmacological and lifestyle modalities, occasionally different device therapy techniques and rarely cardiac transplantation.
In sudden heart failure, the main focus is to ensure enough perfusion and oxygen delivery to vital organs. This involves ensuring that circulation, breathing and airway are sufficient.
For individuals with chronic heart failure, the goal for treatment is to –
- prolong life,
- prevent decompensation of chronic heart failure and
- reducing symptoms creating room for physical activities.
Heart failure can be as a result of different conditions. Controlling and treating the modifiable risk factors and causes are necessary i.e. –
- valves dysfunction,
- hypertension,
- anemia and
- alcohol intake.
Treatment of existing risk factors is normally the initial approach to heart failure treatment. In most heart failure cases, either no underlying cause is found, or treatment of the underlying cause fails to achieve normal heart functioning. In such cases, device and medical treatment methods offer a significant improvement in outcomes, reduced potential death or hospitalization, exercise tolerance and symptoms relief.
The different monitoring methods used to evaluate the progress of individuals undergoing heart failure treatment include bodyweight monitoring and fluid balance.
Remote monitoring can be ideal for reducing complications for individuals with heart failure.
Behavior modification is a major focus in chronic heart failure management program where dietary guideline concerning salt and fluid intake are given.
For individuals with regular admission to hospital or advanced heart failure strategies to prevent readmission such as visiting nurse at home or telephone follow-up are applied.
Conclusion –
Be aware of heart failure symptoms. Seek medical attention if you are having any of the symptom. The earlier medical attention you seek – the lesser in the chance of you getting the complications and progression of the disease.